Asia Pacific J Clin Nutr (1992) 1, 159-168

Trends and dietary implications
of some chronic non-communicable diseases in peninsular Malaysia
Geok Lin Khora PhD and Chong-Ying Ganb
MB BS MPH
aDepartment of Nutrition
and Community Health, University Pertanian Malaysia, 43400 Serdang;
bDepartment of Social and Preventive Medicine,
University of Malaya, 59100 Kuala Lumpur, Malaysia.
Non-communicable diseases with dietary
implications, ischaemic heart disease, diabetes mellitus and cancers
of the breast and colon are discussed in relation to their prevalence
and mortality rates in peninsular Malaysia during the past few decades.
The mortality rate due to diseases of the circulatory system has
more than doubled since 1970, deaths due to ischaemic heart disease
being the major cause. The prevalence of diabetes mellitus has risen
from 0.65% in 1960 to about 4% currently. The mortality risk for
both ischaemic heart disease and diabetes is highest in the Indian
compared to Malay and Chinese populations. The Chinese show the
highest mortality rate for cancers of the breast and colon. This
could reflect, partly, because more people especially in the urban
areas are seeking treatment and improved diagnosis. Empirical dietary
data indicate an increase in the prevalence of hypercholesterolaemia
among urban adults and overweight among urban and rural adults.
Aggregate data from food balance sheets indicate increased availability
of energy intake from fats and oils, sugar, and animal products,
with concomitant decline in available energy from plant products.
Continued public health education on the important linkage between
diet and disease is called for.
Introduction
Economic growth with industrialization
and urbanization in developing countries often brings in its wake
changes in a population's dietary habits. Such dietary changes tend
towards an excess intake of energy-dense foods that are rich in fat
and free sugars, but low in complex carbohydrates38. Evidence
from epidemiological studies has established the link between such
a diet and risk of degenerative chronic diseases of middle and later
adult life, particularly cardiovascular disease and certain types
of cancer13.
Malaysia has undergone remarkable socio-economic
development in recent decades. Its economy has been expanding
rapidly, for example between 1988 and 1990 the gross domestic product
growth averaged about 9% annually. This has led to a rise in its income
per capita from US$334 in 1970 to US$2300 in 1989. Ranked as an upper
middle income country by the World Bank37, Malaysia appears
to be on course like other newly affluent countries in shedding off
'old' problems of undernutrition and infectious diseases for a 'new'
array of challenges posed by increasing incidence of degenerative
diseases such as cardiovascular diseases and neoplasms (Fig. 1).

This paper discusses the prevalences
and mortality trends of selected types of non-communicable diseases
in Malaysia which have dietary implications, namely ischaemic heart
disease, diabetes mellitus, breast cancer and cancer of the digestive
system. The diet-related risk factors of these degenerative diseases
will be discussed in relations to the past and current dietary intake
patterns of Malaysians.
The mortality data presented are based
on medically certified and inspected cases only, which account for
about 40% of the deaths occurring in peninsular Malaysia. Since the
coverage of medically certified and inspected deaths is known to be
more adequate in urban areas, the mortality data tend to have an urban
bias. This article focuses on peninsular Malaysia as reliable data
are less easily available for Sabah and Sarawak. Some comparisons
of the data are presented on the basis of the three main ethnic communities
in peninsular Malaysia, namely Malays, Chinese and Indians.
Ischaemic
heart disease
Since 1970 diseases of the circulatory
system have been the leading cause of deaths in peninsular Malaysia.
In 1989, they contributed to almost 30% of the total certified death
cases, followed by accidents, neoplasms and diseases of the respiratory
system (Table 1). Death due to diseases of the circulatory system
has increased fourfold from 1974 cases in 1965 to 7889 in 1989. In
terms of mortality rates, its incidence has more than doubled between
1970 and 1989 from 24.1 to 55.2 per 100 000 (Table 2). The mortality
rate for diseases of the circulatory system shows a predominance in
the older age groups. For example, the mortality rate for the population
aged between 45-65 years old was 188.2 per 100 000 in 1989, ie 3.4
times higher than that for the general population. The highest frequency
distribution of coronary mortality is reported to have shifted from
the 50-59 age group for both men and women in 1965, to the 60-69 age
group by 198919.
Table 1. The leading causes of
medically certified and inspected deaths in peninsular Malaysia25
.
| Cause
of death |
1989a (%) |
1989 Rank |
1970 Rank |
| Diseases
of the circulatory system |
29.6 |
1 |
3 |
| Accidents,
poisoning and violence |
13.4 |
2 |
4 |
| Neoplasms |
11.8 |
3 |
6 |
| Diseases
of the respiratory system |
8.3 |
4 |
7 |
| Certain
conditions originating in the perinatal period |
7.5 |
5 |
1 |
| Symptoms
of ill-defined and unknown causes |
7.1 |
6 |
2 |
| Infections
and parasitic diseases |
5.5 |
7 |
5 |
| Diseases
of the digestive system |
4.4 |
8 |
8 |
| Diseases
of the genitourinary system |
3.6 |
9 |
10 |
| Congenital
anomalies |
3.0 |
10 |
9 |
a Total of medically certified
and inspected deaths in 1989 was 26 639.
Table 2. Mortality rate of the
main diseases of the circulatory systems in peninsular Malaysia25,26.
| Cause
of mortality |
Mortality rate per 100 000 population |
| |
1970 |
1989 |
| |
45-64 (years) |
All ages |
45-64 (years) |
All ages |
| Diseases
of the circulatory system |
98.2 |
24.1 |
188.2 |
55.2 |
| Ischaemic
heart disease |
na |
na |
75.2 |
22.1 |
| Cerebrovascular
disease |
na |
na |
47.5 |
16 |
na = not available
Among the diseases of the circulatory
system, ischaemic heart disease contributes to a major proportion
of the deaths in this category. In 1989, ischaemic heart disease was
responsible for 38% of the deaths due to diseases of the circulatory
system. It accounted for 11.7% of the total medically certified and
inspected deaths in 1989. This is nearly three times the level in
1970 (4.3%) and the percentage appears to be still on the increase.
The mortality rate for ischaemic heart
disease among the 45-65 age group is about three to four times higher
than that for the population as a whole (Table 2). For all ages, the
ischaemic heart mortality male: female ratio was 2: 125.
This sex mortality ratio in 1989 was higher for the Malays and Indians
at 2.6: 1 compared to 1.4: 1 for the Chinese. Indians in peninsular
Malaysia are at a higher mortality risk for ischaemic heart disease
than the Chinese and Malays (Fig 2). In 1988, the mortality rate for
the Indians was 52.8 per 100 000, ie twice that for the Chinese (26.9)
and four times higher than for the Malays (13.4). A similar finding
was reported for Indians in Singapore whose death rate due to coronary
heart disease was three times higher than that of the Chinese12.
Immigrant Indians in England27, Trinidad28 and
Uganda32 have also been reported to have a relatively high
mortality risk for coronary heart disease.

Diabetes
mellitus
The prevalence of diabetes mellitus in
Malaysia has risen from 0.65% in 1960 to 2.1% in 1981 and is currently
estimated to be about 4%30,31. The prevalence of diabetes
is reported to differ amongst the main ethnic groups. A study in 1966
reported the prevalence of diabetes of Malays, Chinese and Indians
as 1.8%, 4.7% and 4.2% respectively35. A more recent study
of 1996 railway workers found the highest prevalence among Indians
(16.0%) followed by Chinese (4.9%) and Malays (3.0%)18.
These results also point to relatively
higher prevalence rates of diabetes among Malaysians when compared
to the figures for their ethnic counterparts in Singapore (6.1%, 2.4%
and 1.7% for Indians, Malays and Chinese respectively)5.
Similarly high prevalence of diabetes have been reported for Indians
in Fiji (13.3% to 14.8%)11 and for Indians in South Africa
(11.1% to 19. 1%)16
The mortality rate due to diabetes among
Malaysians is on an upward trend albeit gradually since the 1960s.
For all ethnic groups combined and for both sexes, the mortality rate
(for certified deaths only) has risen from 2.19 per 100 000 in 1965
to 3.21 per 100 000 in 1988. During this period the sex differential
in the mortality rates appears to be small, being slightly higher
for women. The mortality rates for men were 1.02 per 100 000 in 1965
and 2.67 per 100 000 in 1988, while the corresponding figures for
women were 1.17 and 2.90 per 100 000 respectively (Fig. 3).
As for ethnic differences, the mortality
rate for Indians has been consistently highest among the three ethnic
groups (7.42 per 100 000 persons in 1988) followed by Chinese (4.77)
and Malays (1.63). However, between 1965 and 1988, the mortality rates
for the latter two groups have increased faster (53% and 71% respectively
for Malays and Chinese) than that for the Indians (10%).
Malignant
neoplasms
In the last two decades, the rate of
mortality due to malignant neoplasms has increased from about 15 to
almost 20 per 100 000 (Table 3). This increase may be due in part
to more people seeking treatment especially with increased urbanization,
improved diagnosis and better reporting. Cancer of the digestive organs
and peritoneum contribute to the largest number of deaths (30.2% in
1989) followed by neoplasms of the respiratory and intrathoracic organs
(23.7%) (Table 4).
Table 3. Rates of medically certified
deaths due to malignant neoplasm in peninsular Malaysia (per 100 000
persons)26.
| 1967-1970
|
14.9 |
| 1971-1975
|
16.4 |
| 1976-1980
|
18.7 |
| 1981-1985
|
19.7 |
| 1986-1989 |
19.9 |
Table 4. Death due to malignant
neoplasm in peninsular Malaysia in 198928.
| Types |
Number of cases |
Per cent of total |
Male: Female ratio |
| Digestive
organs and periotoneum |
910 |
30.2 |
1.9:1 |
| Respiratory
and intra thoracic organs |
714 |
23.7 |
3.0:1 |
| Lymphatic
and haemopoietic tissues |
355 |
11.8 |
1.4:1 |
| Genito-urinary
organs |
281 |
9.3 |
0.3:1 |
| Lip, oral
cavity and pharynx |
264 |
8.8 |
3.1:1 |
| Bone, connective
tissue, skin and breast |
241 |
8.0 |
0.1:1 |
| Other and
unspecified sites |
247 |
8.2 |
1.4:1 |
| Total |
3012 |
100.0 |
1.4:1 |
Colon cancer together with cancers of
the liver and stomach are the main types of cancer of the digestive
organs and peritoneum. The mortality rate due to colon cancer among
the Chinese appear to be increasing gradually from about 3.4 per 100
000 in 1982 to nearly 4.0 in 1988 (Fig. 4). The higher mortality rate
reported for the Chinese as compared to that for the Malays and Indians
could be partly reflective of the higher proportion of Chinese in
the urban population of peninsular Malaysia.
Men have almost twice the mortality risk
of women with regards to cancer of the digestive organs (Table 4).
On the other hand, women encounter a much higher mortality risk with
breast cancer and cancer of the genitourinary organs. The mortality
rate for medically certified cases of breast cancer has been rising
gradually from 1.8 per 100 000 in 1982 to 2.3 per 100 000 in 1988
(Fig. 5). During this period, the Chinese showed the highest mortality
rate from breast cancer reaching 4.2 per 100 000 in 1988, compared
to 2.7 and 1.2 for the Indians and Malays respectively.
Besides cancer of the digestive organs
which have dietary implications, cancer of the oral cavity and pharynx
have also been reported among the Malaysian population and their aetiology
have been linked to dietary factors. In a study of cancer mortality
registered in Kuala Lumpur during 1979-198224, it was found
that nasopharyngeal cancer had a particularly high incidence among
the Chinese, similar to findings in the Chinese community of Hong
Kong, Taiwan, Singapore and China. Genetic predisposition to environmental
factors including long-term consumption of salted fish is hypothesized
to be the underlying aetiological basis1,2. It was also
reported that a high preponderance of deaths due to mouth cancer occurred
among Indians in Kuala Lumpur24. This is believed to be
related to their customary habit of betel nut chewing, especially
among the older age groups.
Diet-related
risk actors of non-communicable diseases
It is well recognized that the association
between diet and disease is very complex. In the case of chronic degenerative
diseases, it is even more difficult to attribute its incidence on
the influence of a specific dietary component because of the long
latent period between the initiation of the disease and the manifestation
of clinical symptoms. Nonetheless, epidemiological and experimental
studies have identified high dietary intake of saturated fat as a
leading cause of high blood cholesterol, which in turn is a high risk
factor of coronary heart diseases. Other recognized risk factors of
coronary heart disease include hypertension, smoking, obesity, diabetes,
stress, high serum uric acid and inactive lifestyle3.
In Malaysia over 95% of diabetic patients
have Type II or non-insulin dependent diabetes (NIDD), which may respond
to diet and weight reduction. An increased incidence of Type II diabetes
is believed to be associated with an increased consumption of refined
carbohydrates and fats and a decreased intake of fibre.
As for the link between diet and cancers
of the breast and colon, evidence particularly from epidemiological
and animal studies suggest that a number of dietary components serve
as promoters of carcinogenesis36. These include saturated
fat, meat and animal protein, nitrate and nitrite; on the other hand,
dietary fibre, vitamin A and/or beta carotene, vitamins C and E and
trace elements such as selenium have been attributed with having protective
capabilities against these cancers.
The following section presents aggregate
data and results of studies that indicate increased prevalences of
hypercholesterolaemia and overweight, and increased availability of
dietary energy from protein and fat sources in Malaysia.
Prevalence
of hypercholesterolaemia
Since the 1960s there have been many
studies determining the blood cholesterol levels of Malaysians. The
mean serum cholesterol level of men aged between 25 to 55 years in
the urban areas was found to be approximately 185 mg/dl in the 1960s22;
by the 1980s, the average cholesterol level of a group of urban executives
and professionals was reported to be about 230 mg/dl33 (Table
5). The latter study identified 31% of the men as hypercholesterolaemic
(cholesterol level exceeding 250 mg/dl). In comparison, in the early
1970s, less than 12% of a group of urban male workers aged 30 and
above were found to be hypercholesterolaemic (level exceeding 200
mg/dl)8.
Among the main ethnic groups, Indians
are reported to have the highest prevalence of hypercholesterolaemia
(43.2%), as compared to 35.2% and 24.2% among the Malays and Chinese
respectively33. Earlier studies8,22 did not
find a significantly higher prevalence of hypercholesterolaemia among
the Indians than the Chinese and Malays (Table 5). This development
is of significance in light of the fact that the Indians presently
show the highest mortality rate for ischaemic heart disease.
Table 5. Mean serum cholesterol
levels among Malaysian men in the urban areas by age and ethnic groups.
| Age
group |
Malays (n) mg/dl |
Chinese (n) mg/dl |
Indians (n) mg/dl |
All races |
Reference |
| 30-39 |
(32)201 |
(38)189 |
(36)174 |
(106)187 |
|
| 40-49 |
(28)185 |
(33)193 |
(33)178 |
(94)185 |
22 |
| 50-59 |
(16)188 |
(26)176 |
(23)175 |
(65)178 |
|
| 30-39 |
(56)203 |
(102)197 |
(38)192 |
(196)198 |
|
| 40-49 |
(46)228 |
(52)206 |
(34)216 |
(132)216 |
8 |
| 50-59 |
(21)237 |
(21)232 |
(15)217 |
(57)230 |
|
| 25-34 |
|
|
|
(146)224 |
|
| 35-44 |
|
|
|
(209)236 |
|
| 45-54 |
|
|
|
(51)239 |
33 |
| 55-64 |
(176)236 |
(182)227 |
(37)247 |
(406)232 |
|
Communities living in the rural areas
have been found to have a lower average serum cholesterol level than
their urban counterparts. The mean blood cholesterol level for the
aborigines in west Malaysia was found to be low at about 156 mg/dl
and none of them were hypercholesterolaemic4. The average
cholesterol level among poor rural Malay men was reported to be also
low, at 175 mg/ dl9.
Prevalence
of overweight
A number of studies have reported on
the increased prevalence of overweight among Malaysians based on the
definition of body mass index (BMI) exceeding 25 kg/m2
as overweight. Among urban subjects it was found that, on average,
one quarter to one third of the men and women studied were overweight17,33
(Table 6). In a study of a rural low income Malay community, 45.5
% of 134 men and 43.1 % of 153 women studies were found to be overweight15.
The prevalence of overweight was found to increase with age for both
men and women. In comparison, previous studies of poor Malay rural
subjects had found a low prevalence of overweight. For example, in
16 villages studied in 1979-1983, it was found that only 5% of 522
men and 15% of 956 women aged 18 years and above were overweight9.
Table 6. Prevalence of overweight
among Malaysians as indicated by body mass index (BMI).
| Age (years) |
Number |
Community |
Gender |
Prevalence of obesity (%) |
Criteria for overweight |
Reference |
31-40
41-50 |
300 |
urban |
male |
44% Malays
4% Chinese
24% Indians
20% Malays
20% Chinese
27% Indians |
BMI>21.5 male
BMI>20.5 female |
17 |
31-40
41-50 |
300 |
urban |
female |
20% Malays
7% Chinese
50% Indians
33% Malays
20% Chinese
27% Indians |
|
17 |
| 18+ |
522
965 |
poor rural Malays |
male
female |
5%
15% |
BMI>25 male BMI> female |
9 |
| 18+ |
134
153 |
rural mixed ethnicity |
male
female |
46%
43% |
BMI= 15-29.9 male and female |
15 |
25-34
35-44
45-54 |
146
209
51 |
urban executives mixed ethnicity |
male |
26.2%
29.3%
33.3% |
BMI= 25-30 |
33 |
Overweight is known to contribute to
high serum lipid levels. Such a positive association was shown among
Malaysian subjects who were overweight (BMI above 25), and they had
higher levels of triglycerides and total cholesterol, and a significantly
lower level of high-density lipoprotein cholesterol than the non-overweight
subjects10.
Increased
availability of dietary energy
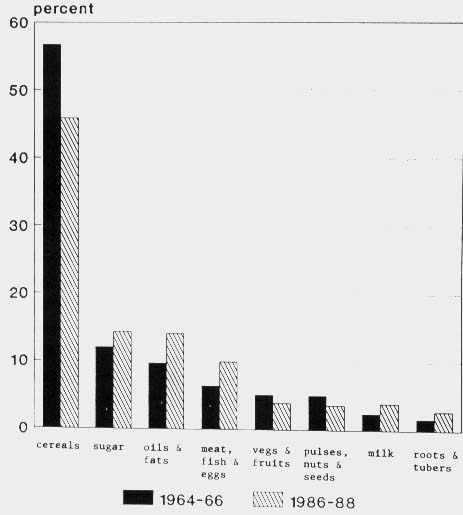
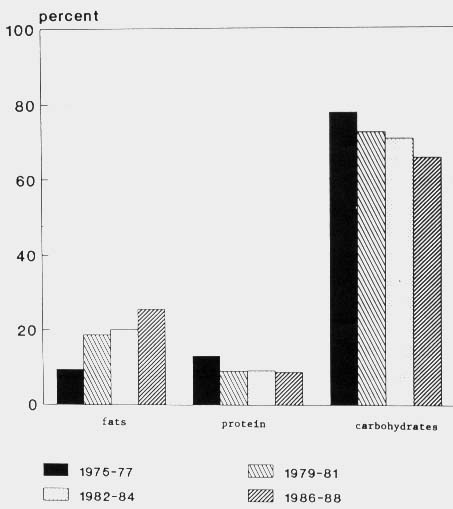
Based on data from the food balance sheets
from 1965-1966 to 1986-1988, it is shown that Malaysians presently
have available 21% more dietary energy per capita per day than two
decades ago21. The increase in available dietary energy
has been towards more energy from oils and fats, animal products and
sugar (Fig. 6).
Figure 6. Changes in sources of
calories in Malaysia between 1964-66 and 1986-8l4.
Energy intake from animal products, particularly
chicken and eggs, has increased from 6.4% of the total available in
1964-1966 to 9.9% in 1986-1988. This has given rise to an increase
in total animal fat available from 16.4 grams per capita per day in
1964-1966 to 24.8 grams in 1986-1988. In terms of protein availability
(grams per capita per day), the amount of chicken and eggs available
have increased five and three times respectively during the two decades
mentioned.
As for cooking oils and fats, there has
been a substantial shift since the 1960s from the use of coconut oil,
a highly saturated oil to palm oil which has a higher content of unsaturated
fatty acid. Palm oil together with palm kernel oil contributed to
40.7% of the total available fat in 1986-1988.
Energy from sugar constituted 14.3% of
the total in 1986-1988, and its availability at 107 grams per capita
per day places Malaysia among the highest users in the ASEAN region20.
The food balance sheets are more likely
to reflect the consumption patterns of the urban and upper income
groups. This is indicated by past dietary studies which reported a
much lower mean nutrient intake per capita in low income households
than the average levels shown in the food balance sheets. For example,
the mean energy intake averaged about 1900 kcal (8mJ) per capita per
day among the rural poor and about 1400 kcal (5.9 mJ) for urban
squatters, compared with the mean availability figure of 2665
kcal (11.2 mJ) per capita in the 198~88 food balance sheet. The levels
of energy intake by urban middle to upper income groups come closer
to the food balance sheet level (Table 7).
Table 7. Dietary energy per capita
intake levels of rural and urban communities in Malaysia.
| Community |
Mean intake kcal (MJ) |
Mean intake as % of RDI (range)a |
Number of households |
Reference |
1. Rural
communities in Sabah:
Murut
Upland Kadazan
Coastal plain Kadazan
Chinese |
|
153 (71-263)
86 (47-159)
103 (75-152)
83 (42-98) |
99 |
7 |
| 2. Poverty
rural villages |
1874 (7.87) |
90 (70-101) |
503 |
9 |
| 3. Rural
and urban combined. mostly Malays |
2297 (9.65) |
110 |
1219 |
39 |
4. Urban
Rural |
2162(9.08)
1988(8.35) |
110 |
100 |
29 |
5. Urban
squattersb
Malays
Chinese
Indians |
1412 (5.93)
1433(6.02)
1383(5.81) |
63
64
61 |
114b
63b
86b |
|
a RDI for Malaysians35;
bindividuals (as opposed to households)
While the availability of energy from
sugar, animal products, and oils and fats has been on the upward trend,
there has been a concomitant decline in the dietary energy from cereals
and other plant products. The contribution from plant products has
dropped from 56.7% of total energy intake in the l960s to 45.9% currently.
Meanwhile, the proportion of dietary energy from other plant products
like pulses, nuts and oilseeds, fruits and vegetables has decreased
too. The significance of this trend is related to the protective effects
of plant foods such as cruciferous vegetables on colorectal cancer23.
Overall, the food balance sheets indicate
a dietary trend in Malaysia that is tending towards a decreasing proportion
of energy intake from complex carbohydrates and a rising proportion
from edible oils and fats and protein from animal sources (Figs 6,
7).
Figure 7. Changes in composition
of calories from protein, fat and carbohydrates14.
Conclusion
In Malaysia studies pertaining to diet-related
noncommunicable diseases are limited to reports on the prevalence
of their risk factors, and epidemiological data based on mortality
statistics, and hospital admissions and registration. Owing to the
rapidly expanding economy in recent decades. Malaysia has undergone
extensive socio-economic development. Among the effects of development
is the influence on lifestyle behaviour of Malaysians particularly
the affluents in urban areas. Lifestyle behaviour related to diet,
smoking, socio-emotional stress, intake of 2 alcohol and physical
activity are important risk factors of degenerative diseases
such as ischaemic heart diseases. Examining the mortality figures
based 3 on certified and inspected deaths which are more reflective
of the urban population, there appears to 4 be a rise of these diseases
especially amongst the Indians. At the macro level, dietary data indicate
in 5 general a higher intake of animal products and edible oils and
fats and lower consumption of fruits, vegetables and legumes. There
is a need for in-depth 6 studies on the lifestyle determinants
of the different ethnic groups, especially of the Indian community,
in order to obtain a better understanding of the ethnic differentials
in the prevalences and mortality rates of the non-communicable diseases
that have emerged in Malaysia. It is timely that the Malaysian government
has in recent years conducted an active public campaign on healthy
lifestyles, with emphasis directed towards dietary moderations. With
increased public awareness of the importance of diet that is consistent
with good health, the current rising advance of noncommunicable diseases
in Malaysia may be checked and a major problem for public health forestalled.
Acknowledgement - Appreciation is extend to GM Tang and SN Lee in the Department
of Social and Preventive Medicine, University of Malaya for their
technical assistance. The secretarial help of Chelvi Shanmugam is
much appreciated.
References
- Armstrong RW, Armstrong MJ, Yu MC,
Henderson BE. Salted fish and inhalants as risk factors for nasopharyngeal
carcinoma in Malaysian Chinese. Cancer Research 1983; 43:29~57-2970.
- Armstrong RW, Chan SE. Salted fish
and nasopharyngeal carcinoma in Malaysia. Soc Sci Med 1983; 17:1559-1567.
- Barna M, Biro G. Atherosclerosis:
dietary considerations. World Rev Nutr Diet 1989; 59:126-155.
- Burns-Cox, CJ, Chong YH, Gilman R.
Risk factors and the absence of coronary heart disease in aborigines
in West Malaysia. Br Heart J 1972; 34:953-958.
- Cheah, JS, Yeo PPB, Lui KF, Tan BY,
Tan YT, Ngu YK. Epidemiology of diabetes in Singapore. Med J Malaysia
1982; 37:141-149.
- Chee, HL. Nutrient intake levels in
an urban squatter community. Proc Nutr Soc Malaysia 1989; 4:25-34.
- Chen, PCY, Chan, MKC, Teoh, ST et
at. A nutrition study of he interior, west coast and Kudat Divisions
of Sabah. Kuala Lumpur: University of Malaya, 1981.
- Chong YH. Khoo KL. Serum lipid levels
and the prevalence of hyperlipidaemia in Malaysia. Clin Chim Acta
1975; 65:143-148.
- Chong YH, Tee ES, Ng TKW et al. Status
of community nutrition in poverty kampungs. Bulletin No. 22. Kuala
Lumpur: Institute for Medical Research, 1984.
- Chong YH, Ng TKW. Association of obesity
with serum lipid and lipoprotein levels. ASEAN J Clin Sci 1985;
:124-126.
- Ekoe, JM. Diabetes mellitus, aspects
of the world-wide epidemiology of Diabetes mellitus and its long
term complications. Amsterdam: Elsevier Science Publishers, 1988.
- Emmanuel SC. (1989). Trends in coronary
heart disease mortality in Singapore. Sing Med J 1989; 30:17-23.
- Evers S. Diet-disease relationships:
public health perspectives. Progress Food Nutr 1991; 15:61-83.
- Food and Agriculture Organisation.
Food Balance Sheets, 1964-1966 to 1986-1988. Rome: Food and Agriculture
Organisation.
- Hakwelele L, Somarsono N, Phanthaly
P. Community diagnosis: factors influencing the prevalence of adult
overweight in the low cost housing project of Tanjong Karang, Kuala
Selangor. Master of Community Nutrition Thesis. Kuala Lumpur: University
Kebangsaan Malaysia, 1991.
- Jackson WPU. Epidemiology of diabetes
in South Africa. Adv Metabolic Disorders 1978; 9:111-146.
- Jones JJ. A comparative study of the
prevalence of adult obesity in the three racial groups of Kuala
Lumpur. Med J Malaysia 1976; 30:256-260.
- Khalid BAK, Rani R, Ng ML, Kong CT,
Tariq AR. Prevalence of diabetes, hypertension and renal disease
amongst railway workers in Malaysia. Med J Malaysia 36 1990; 45:8-13.
- Khoo KL, Tan H, Khoo TH. Cardiovascular
mortality in Peninsular Malaysia. Med J Malaysia 1991; 46:7-20.
- Khor GL, Tee ES, Kandiah M. Patterns
of food production and consumption in the ASEAN region. World
Rev Nutr Dietet 1990; 61: 1-40.
- Khor GL. Dietary patterns of Malaysians:
nutritional and 39 health implications. ASEAN Food J 1991; 6:52-57.
- Lau KS, Lopez CG. Gan OM. Serum cholesterol
levels in Malays, Indians and Chinese in Malaya. Med J Malaysia
1962; 16:184-192.
- Lee HP. Diet and cancer - some results
from Singapore. Asia Pacific J Clin Nutr 1992, 1 :43-46.
- Lim HH. Cancer mortality in the Federal
Capital of Malaysia. Singapore Med J 1986; 27:512-518.
- Malaysia Department of Statistics.
Vital Statistics Peninsular Malaysia 1968-1989. Kuala Lumpur: Department
of Statistics Malaysia.
- Malaysia Ministry of Health. Annual
Reports 1980-1989. Kuala Lumpur: Ministry of Health Malaysia.
- Marmot MG, Adelstein AM, Bulusu L.
Lessons from the study of immigrant mortality. Lancet 1984; i:1455-1458.
- Miller GH, Beckles GLA, Alexis SD,
Bynam NTA, Price SGL. Serum lipoproteins and susceptibility of men
of Indian descent to coronary heart disease. The St James Survey,
Trinidad. Lancet 1966; 2:332-333.
- Mohamed GM, Siti KS. Food availability
and patterns of food intake. Presented at Seminar on Food Security
and Policy issues. Universiti Pertanian Malaysia, Serdang, July
1986.
- Mustafa BE. Diabetes mellitus in Peninsular
Malaysia: ethnic differences in prevalence and complications. Annals
of the Academy of Medicine 1985; 14:272-276.
- Mustafa BE. Diabetes in Malaysia:
problems and challenges. Med J Malaysia 1990; 45: 1-7.
- Sharper AG, Jones KW. Serum cholesterol,
diet and coronary heart disease in Africans and Asian in Uganda.
Lancet 1959; 2:534-537.
- Teo PH, Chong YH, M. Zaini AR. Coronary
risk factors among Malaysian male executives in two urban areas.
Proc Nutr Soc Malaysia 1988; 3:24-31.
- Teoh ST. Recommended daily dietary
intakes for Peninsular Malaysia. Med J Malaysia 1975; 30:38-42.
- West KW, Kalbfleisch JM. Glucose tolerance,
nutrition and diabetes in Uruguay, Venezuela, Malaysia and East
Pakistan. Diabetes 1966; 15:9-18.
- Willet W. The search for the causes
of breast and colon cancer. Nature 1989; 338:389-394.
- World Bank World. Development Report
1988. New York: Oxford University Press, 1988.
- World Health Organisation. Diet, nutrition,
and the prevention of chronic diseases. WHO Technical Report Series
No. 797. Geneva: WHO, 1990.
- Zanariah J, Jaafar R. Othman, Abdullah
NR. Studies of the food intake trend of the population in urban
and rural areas in four selected districts in West Malaysia. Malaysian
Agriculture Research and Development Institute (MARDI) Report No.
106. MARDI, Serdang, 1986.
Trends
and dietary implications of some non-communicable diseases in peninsular
Malaysia
Geok Lin Khor and Chong-Ying
Gan
Asia Pacific Journal of
Clinical Nutrition 1992; 1:159-168.
Telah dibahas angka prevalensi dan mortalitas
penyakit-penyakit degeneratif khronis seperti penyakit jantung iskhemik,
diabetes mellitus, kanker payudara dan usus besar dengan implikasi
dietnya di Peninsular Malaysia selama beberapa dekade terakhir. Angka
mortalitas akibat penyakit-penyakit sistim sirkulasi meningkat lebih
dari dua kali lipat sejak 1970 dan kematian akibat penyakit jantung
iskhemik merupakan penyebab utama. Angka prevalensi diabetes mellitus
telah meningkat dari 0.65% pada tahun 1960 menjadi 4% akhir-akhir
ini. Resiko mortalitas penyakit jantung iskhemik dan diabetes mellitus
dietmukan tertinggi pada etnik India bila dibandingkan dengan etnik
Melayu dan Cina. Etnik Cina menunjukkan angka mortalitas kanker payudara
dan usus besar tertinggi. Keadaan ini merupakan refleksi perkembangan
diagnosa akibat semakin meningkatnya kesadaran orang-orang kota mencari
pengobatan. Data diet secara empirik menunjukkan peningkatan prevalensi
hiperkolesterolemia di antara orang-orang kota dan pedesaan. Data
pola makan menunjukkan peningkatan penggunaan kalori dari lemak dan
minyak, gula dan produk-produk hewan, disertai dengan penurunan penggunaan
kalori dari produk-produk tumbuhan. Kesinambungan pendidikan kesehatan
masyarakat tentang pentingnya hubungan antara diet dan penyakit adalah
tepat.
Copyright © 1992 [Asia Pacific Journal of Clinical
Nutrition]. All rights reserved.
Revised:
January 19, 1999
.
to the top